As we settle into month two of lockdown, we are starting to see the impact of these measures on physical activity and therefore health

Whilst key workers continue to face immense challenges, those of us at home can play our part in protecting the NHS from a influx of conditions related to inactivity after the restrictions are eased.
Has lockdown changed our physical activity levels?
The repercussions of lockdown are only just beginning to be understood. It is challenging at the best of times to get an accurate measure of physical activity at population level, and a sudden and extreme change adds further complexity. However, researchers have been scrambling to capture data and early reports are starting to be shared. Viewed collectively they can inform our understanding of the situation.
It would be easy to think that lockdown might actually lead to increased levels of physical activity and that the Government guidance might encourage people to exercise on a daily basis. But the emerging data suggests otherwise.
Observationally at the start of lockdown, people were suddenly exercising more visibly. This could have been due to no indoor exercise facilities, no organised sport, fortuitous good weather etc. Whatever the reason, we saw more people cycling, walking and running than ever before. However, UK data released after two weeks of lockdown based on self-reported physical activity levels from 45,000 people paint a mixed picture. One in four reported not exercising during the week and people with mental and physical health conditions were doing the least physical activity. Older adults were doing more gentle exercise like walking than other age groups but doing the least exercise at home or moderate/high intensity exercise outside the home. And people living alone and those with lower household income reported also engaging less in all kinds of physical activity.
A further data set from Sport England suggests that there is enhanced recognition of the importance of physical activity as a result of the pandemic and that many people were using exercise to help manage their health during this period. However, it also showed that 41% reported doing less activity than before lockdown and that those with a longstanding condition or illness were less likely to be regularly active than those with no longstanding condition or illness.
While a clearer picture will emerge over time, the early findings suggest that existing inequalities in physical activity levels persist and may be further compounded by lockdown.
What does this mean for our health and wellbeing?
Physical activity is critical for mental and physical wellbeing and prolonged periods of reduced activity will have a significant impact. This could lead to increased demand for medical treatment when the NHS needs to focus on the various repercussions of lockdown and Covid-19.
Physical activity is a key way for many people with existing health conditions to manage their symptoms, without it they may experience increased pain and stiffness and reduced mobility. As healthcare resources are stretched, we need to support people to self-manage as well as possible.
We are in an unprecedented pandemic situation; it is a stressful and uncertain time. Physical activity is a critical mechanism to manage mental health for everyone, particularly for people with existing mental health conditions. Evidence suggests that sedentary behaviour can increase depressive symptoms in healthy adults after as little as seven days, and that it has a protective effect against developing anxiety.
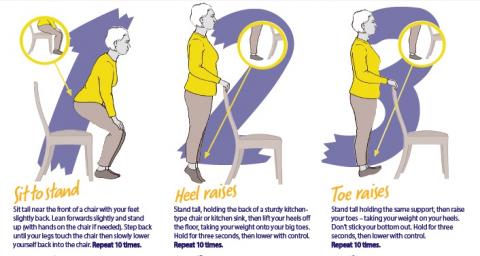
Multiple weeks of reduced activity could result in substantial physical deconditioning, affect day-to-day functioning, and the independence of many people. This can lead to falls and fractures which can have a devastating impact on quality of life, and which of course have substantial health and social impacts.
Many people are also experiencing interruptions in NHS care as a result of coronavirus. Appointments may be postponed, diagnostics delayed and elective surgery postponed. Finding ways to stay active during disrupted care will help to manage ongoing symptoms such as pain, maintain function, and help manage anxiety through these difficult times.
Why we need to stay active
Alongside the immediate rehab needs of people who have had coronavirus, we are likely to see a wider impact on population health as a result of lockdown, in part due to reduced physical activity levels.
There is a risk that physios will be inundated with people who have aches and pains as a result of inactivity and sedentary behaviour.
Physiotherapists have a role in supporting people to stay active, particularly those who face barriers to activity, for example those with mental or physical health conditions.
In the UK, a report suggests that two thirds of people who have fallen seriously ill with coronavirus were overweight or obese. Almost 72% of those admitted to critical care with coronavirus were overweight, including 40% who were obese. Obesity can cause a range of health conditions, which may make the virus more deadly. In addition, it can exacerbate breathing problems.
During lockdown we need to be more creative about activity. We should see this as an opportunity to be more active rather than less and help the NHS. There’s key guidance on physical activity and an abundance of online information to get started.
The vast majority of us are being responsible in terms of social distancing but we also need to take charge of our health too, and do our bit to look after ourselves, our family and ultimately the NHS.
Dr Anna Lowe is the Programme manager at The National Centre for Sport & Exercise Medicine, Sheffield. @annalowephysio
Find Out More
Number of subscribers: 2