Luke Rendell and Maxine Hoole set out one hospital’s policy on dealing with complex tracheostomy in prolonged disorders of consciousness.
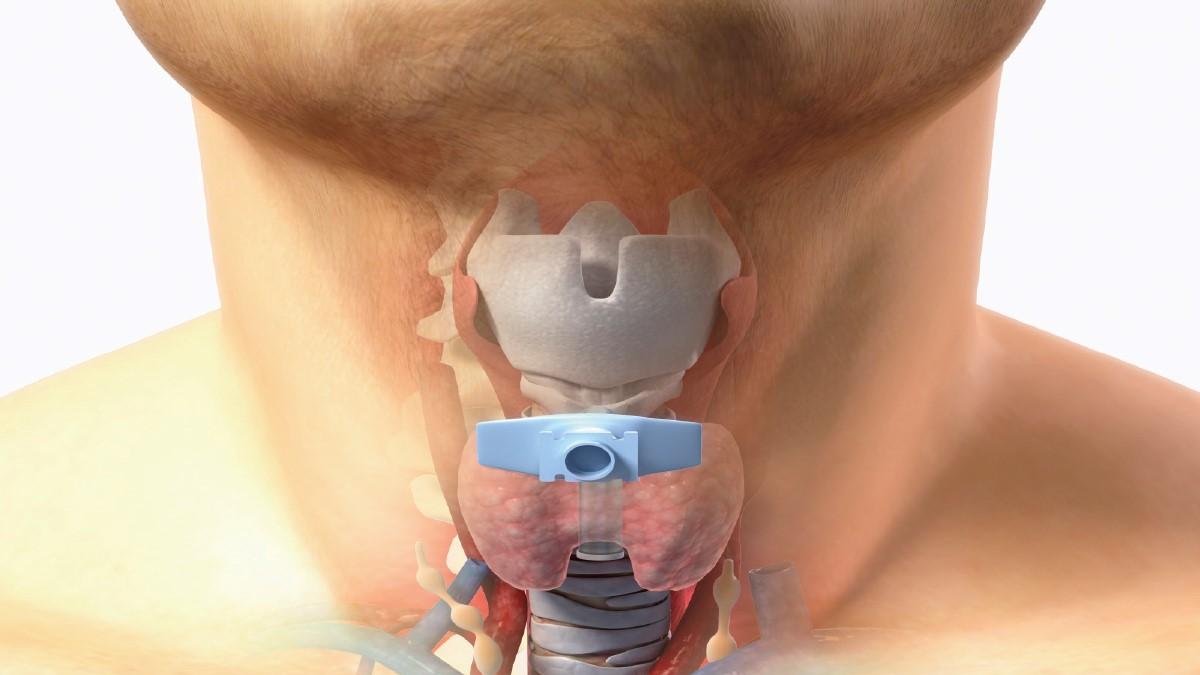
A prolonged disorder of consciousness (PDOC) is a state of altered consciousness and awareness persisting for more than four weeks following a profound brain injury. Many patients will progress through the stages of coma, vegetative state and minimally conscious state as they emerge to full awareness, but some will remain in a vegetative state or minimally conscious for the rest of their lives. Many patients with severe brain injury require a tracheostomy to protect their airway and facilitate weaning off a ventilator. Those who remain in PDOC require the tracheostomy on a long-term basis and can be complex to wean.
The Royal College of Physicians (RCP) published national clinical guidelines on the diagnosis and management of patients with PDOC in 2013.The RCP PDOC guidelines recommend that airway management and tracheostomy care should be included in multidisciplinary goal-orientated programmes of care for all patients in a prolonged disorder of consciousness.
The Royal Hospital for Neuro-disability (RHN) provides a range of services including specialist assessment, treatment and disability management for adults with profound brain injuries. We have a large number of tracheostomy patients spread across our level 1 rehabilitation pathway and continuing care services. At any one time we can have up to 50 patients with tracheostomies, all of whom come into contact with a wide variety of healthcare professionals, support workers and volunteers. We pride ourselves on complex tracheostomy weaning and long-term management, and strive to provide an environment that is safe for patients with a tracheostomy so they can have the same opportunities as those without.
At the RHN we recently conducted a complete review of our tracheostomy care guidelines and policy. This overhaul was performed to reflect the best practices we use to manage neurological patients who are complex to wean or have long-term tracheostomies, an area in which there is little clinical evidence.
Physiotherapy took a strong lead in this process due to practitioners’ broad skill set and knowledge in the areas of respiratory management and tracheostomy care, but it was very much a multidisciplinary team process with significant contributions from speech and language therapists, respiratory nurses and rehabilitation consultants.
Strict training programme
The new tracheostomy policy and guidelines draw on knowledge and experience from a number of sources, including the St George’s tracheostomy policy, other local NHS hospital trust guidelines and the 2013 National Tracheostomy Safety Project. The guidelines also strongly reflect recommendations set out in the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Tracheostomy Care: On the Right Trach? (2014).
Due to the high number of tracheostomy patients at RHN, a variety of tubes being used and various stages of weaning, it is essential that all staff members caring for patients with tracheostomies are confident and possess the required skills and knowledge. In order to ensure this standard of care, a strict training programme was designed, encompassing three levels of competencies.
All staff are required to attend the appropriate level of training and then must have their competencies signed off by their immediate supervisor on the ward. Tracheostomy competencies are considered standard practice across many hospitals, but in order not to limit our patients to the ward environment, our level one training is designed for those who are typically unfamiliar with tracheostomies.
Examples of this are:
- accessing a quiet one-to-one space with a psychologist for assessment/treatment;
- kitchen assessments with the occupational therapists;
- attending music therapy groups or accessing the hospital gardens.
See Table 2 for topics covered.
Tracheostomy champions
During the review, it was also highlighted that as physiotherapists are key in tracheostomy weaning and also have skills in respiratory management, they should possess the skills to change and decannulate tracheostomy tubes in both routine and emergency situations. With the support of the RHN respiratory nurse and the critical care nurse consultant from St George’s Hospital, physiotherapists with extensive tracheostomy experience were trained to be the hospital’s ‘tracheostomy champions’. This included the completion of level 3 competencies (see table 2) and taking on an active role in teaching and training. The tracheostomy champions became responsible for assessing and ‘signing-off’ other clinical staff members on their competencies.
A multidisciplinary peer support programme was also set up between the tracheostomy champions, speech and language therapists, specialist nurses and doctors, to allow sharing of knowledge and experience around complex weaning, providing time to discuss topics such as optimisation of secretion and saliva management, humidification and complex weaning goals.
The next stage is to conduct a number of clinical audits looking at: adherence to completion of the mandatory competencies, current clinical practice against the new policy and guidelines and decannulation success rates. We are also in the process of rolling out e-learning modules for level 1 and 2 competencies, which are to be completed by all staff annually. We plan to conduct research to look for trends or early predictors to successful decannulation among people with PDOC.
- Luke Rendell and Maxine Hoole are physiotherapists in, respectively, neuro-rehabilitation and respiratory care at the Royal Hospital for Neuro-disability in London.
Table 1: Barriers to tracheostomy weaning in PDOC
- low level of consciousness
- structural airway issues (trauma, tracheal malacia, hyper-granulation)
- immobility
- absent cough or impaired cough
- absent or impaired swallow
- dysautonomia
- impaired central respiratory control (abnormal breathing patterns)
Table 2: RHN competencies
- Level 1 (healthcare assistants, doctors, occupational therapists, psychologists, music therapists, therapy support staff) Basic airway anatomy, knowledge of tube components, signs of respiratory distress, how and who to call for help in emergency situations, Yankauer suctioning (optional).
- Level 2 (all nurses, physios and speech and language therapists) Suctioning, basic humidification and emergency management.
- Level 3 (senior nurses and physios) Complex weaning, decannulation and changing, advanced humidification, advance life support.
References
- NCEPOD On the Right Trach? (2014) A review of care received by patients who had a tracheostomy
- UK National Tracheostomy Safety Project (2013)
- St George’s University Hospitals (2000) tracheostomy guidelines
Author
Luke Rendell and Maxine Hoole
Number of subscribers: 3
